The "Chinese Cervical Cancer Screening Guidelines (Part 1)" were jointly developed by seven major domestic professional associations, including the Chinese Society of Reproductive Medicine Vaginoscopy and Cervical Pathology Branch, the Chinese Medical Association Gynecologic Oncology Branch, etc. The guidelines were compiled by national experts and aim to clarify the purpose of cervical cancer screening in China. They establish methods suitable for the Chinese context, identify target populations for screening, and provide guidance principles for screening special populations. Following the principles of evidence-based medicine, the guidelines present recommended practices and levels for cervical cancer screening. The goal is to offer a foundation for clinical practitioners and healthcare professionals involved in cervical cancer prevention and treatment, thereby enhancing the management standards of cervical cancer screening.
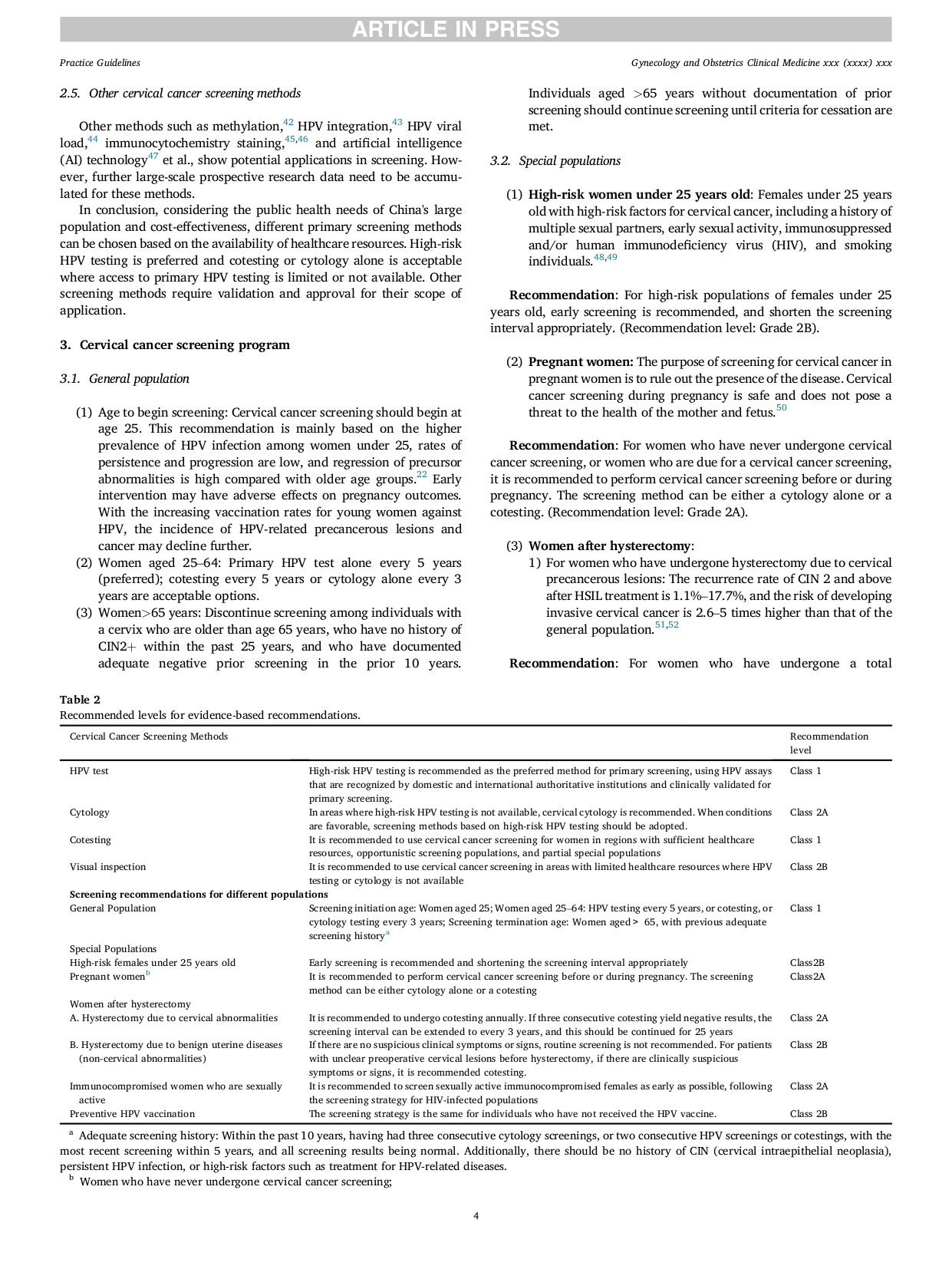
- Cervical Cancer Screening Methods:
Recommendation 1:
High-risk HPV nucleic acid testing is recommended as the preferred method for primary screening. Approved methods and reagents for HPV nucleic acid testing, validated clinically for primary screening, are recommended. (Recommendation level: Class 1).
Using PCR-based HPV testing to examine vaginal self-sampling samples can yield screening sensitivity equivalent to that of samples collected by clinicians.[25] Due to the advantages of convenience, privacy protection, and cost savings, self-sampling screening has been widely implemented worldwide and incorporated into government-led cervical cancer screening programs covering the entire population in multiple countries and regions. [14] Large-scale studies have also been conducted in China. [25–26]
Recommendation 2:
In areas where high-risk HPV testing is not available, cervical cytology is recommended. When conditions are favorable, screening methods based on high-risk HPV testing should be adopted. (Recommendation level: Class 2A).
Recommendation 3:
It is recommended to use co-testing for women in regions with sufficient healthcare resources, opportunistic screening populations, and certain special populations. (Recommendation level: Class 1).
Recommendation 4:
It is recommended to use VIA/VILI as cervical cancer screening in areas with limited healthcare resources where HPV testing or cytology is not available. (Recommendation level: Class 2B).
Other Cervical Cancer Screening Methods:
Methods such as methylation,[42] HPV integration, [43] HPV DNA load,[44] immunocytochemical staining,[45–46] and artificial intelligence (AI) technology [47] et al., show potential applications in screening. However, further large-scale prospective research data need to be accumulated for these methods
- Cervical Cancer Screening Protocol
Screening Protocol:
1. Age to begin screening
Cervical cancer screening should begin at age 25. This recommendation is mainly based on the higher prevalence of HPV infection among women under 25, rates of persistence and progression are low, and regression of precursor abnormalities is high compared with older age groups.[22] Early intervention may have adverse effects on pregnancy outcomes. With the increasing vaccination rates for young women against HPV, the incidence of HPV-related precancerous lesions and cancer may decline further.
2. Women aged 25–64
Option 1: Primary HPV test alone or co-testing every 5 years;
Option 2: Cytology alone every 3 years.
3. Women>65 years
Discontinue screening among individuals with a cervix who are older than age 65 years, who have no history of CIN2+ within the past 25 years, and who have documented adequate negative prior screening in the prior 10 years.
Individuals aged >65 years without documentation of prior screening should continue screening until criteria for cessation are met.
Cervical Cancer Screening for Special Populations
Recommendation 1:
For high-risk populations of females under 25 years old, early screening is recommended, and shortening the screening interval is appropriate. (Recommendation level: Class 2B).
Recommendation 2:
For women who have never undergone cervical cancer screening or women who are due for a cervical cancer screening, it is recommended to perform cervical cancer screening before or during pregnancy. The screening method can be either a cytology alone or a co-testing. (Recommendation level: Class 2A).
Recommendation 3:
For women who have undergone a total hysterectomy due to cervical abnormalities, it is recommended to undergo co-testing annually. If three consecutive co-testing yields negative results, the screening interval can be extended to every 3 years, and this should be continued for 25 years. (Recommendation level: Class 2A).
For patients with unclear presence of precancerous lesions before surgery, if there are clinically suspicious symptoms or signs, co-testing is recommended. (Recommendation level: Class 2B).
Recommendation 4:
It is recommended to screen sexually active immunocompromised females as early as possible, following the screening strategy for HIV-infected populations. (Recommendation level: Class 2A).
Recommendation 5:
Individuals who have received the HPV vaccine should still follow age-specific screening recommendations(same as unvaccinated individuals). (Recommendation level: Class 2B).

- Attached: Original Text of the Guidelines